A team of international researchers, including a mathematical modeller from the Oxford Martin School’s Programme on Emerging Infections, has found that HIV is still replicating in the lymphoid tissue, even when it is undetectable in the blood of patients on antiretroviral drugs.
The study, led by Northwestern University, USA, is published in the journal Nature and its findings provide a critical new perspective on how HIV persists in the body despite potent antiretroviral therapy.
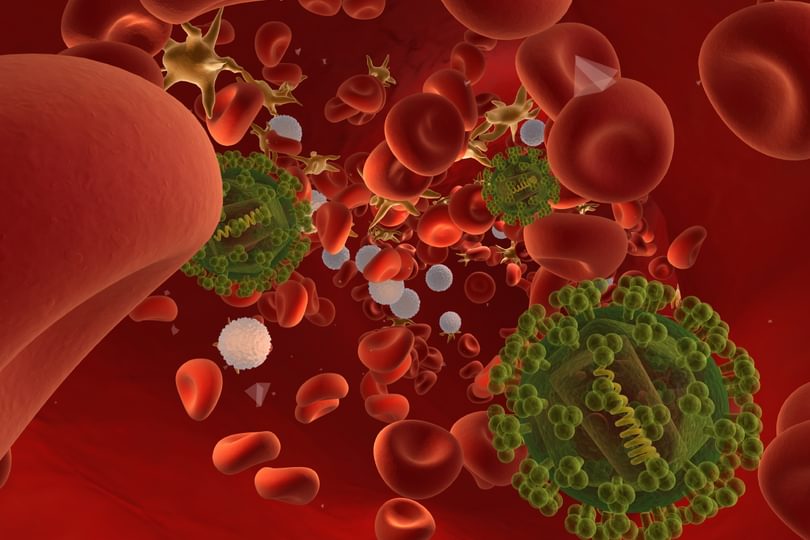
Antiretrovirals, infected cells and the lymphatic system
Combinations of potent antiretroviral drugs quickly suppress HIV to undetectable levels in the bloodstream of most patients, but HIV remains in a viral reservoir within lymphoid tissue in the body. If patients stop taking their drugs, the virus rapidly rebounds in the blood.
Up until now, most scientists believed that the reservoir contains only long-lived infected cells in a resting state, rather than newly infected cells. No-one had seen viruses with new genetic mutations, which arise when HIV completes cycles of growth. In addition, most patients do not develop the drug resistant mutations that might seem likely if HIV were growing in the presence of drugs.
The team examined viral sequences in serial samples of cells from lymph nodes and blood from HIV-infected patients who had no detectable virus in their blood. Scientists found that the viral reservoir was, in fact, constantly replenished by low-level virus replication in lymphoid tissue, with infected cells then moving from these protected sanctuaries into the blood.
Because infected cells in drug-sanctuaries within lymphoid tissue can still produce new viruses, infect new target cells and replenish the viral reservoir, it has not been possible to purge the body of latently infected cells and eradicate the virus.
A mathematical model, developed by Dr Helen Fryer of the Oxford Martin School, tracked the amount of virus and the number of infected cells as they grew and evolved in drug sanctuaries before moving through the body. The model explains how HIV can grow in drug sanctuaries in lymphoid tissue where antiretroviral drug concentrations are lower than in the blood, and why viruses with mutations that create high-level drug resistance do not necessarily emerge.
Implications
The findings provide a new perspective on how HIV persists in the body despite potent antiretroviral therapy. The study also explains why the development of drug resistance is not inevitable when virus growth occurs in a place where drug concentrations are very low.
Most importantly, this new understanding highlights how important it is to deliver high concentrations of antiretroviral drugs to all locations in the body where HIV can grow. Drugs that penetrate the newly discovered sanctuaries will be a prerequisite to the elimination of the viral reservoir and, ultimately, a step towards a cure.
‘The study is exciting because it really changes how we think about what is happening in treated patients,’ said co-author Professor Angela McLean, Professor of Mathematical Biology at Oxford University and Director of the Oxford Martin Programme on Infectious Diseases, who supervised the mathematical modelling. ‘It helps explain why some strategies that tried to clear the reservoir have failed.’
Dr Helen Fryer added: ‘By learning more about how HIV continues to exist within treated individuals, we are one step closer to finding a cure.’
“The challenge now is to deliver drugs at clinically effective concentrations to the location in the patient’s system where the virus continues to replicate,” concluded corresponding author Dr Steven Wolinsky, chief of infectious diseases at Northwestern University Feinberg School of Medicine and a Northwestern Medicine physician.
Nature: Persistent HIV-1 replication maintains the tissue reservoir during therapy